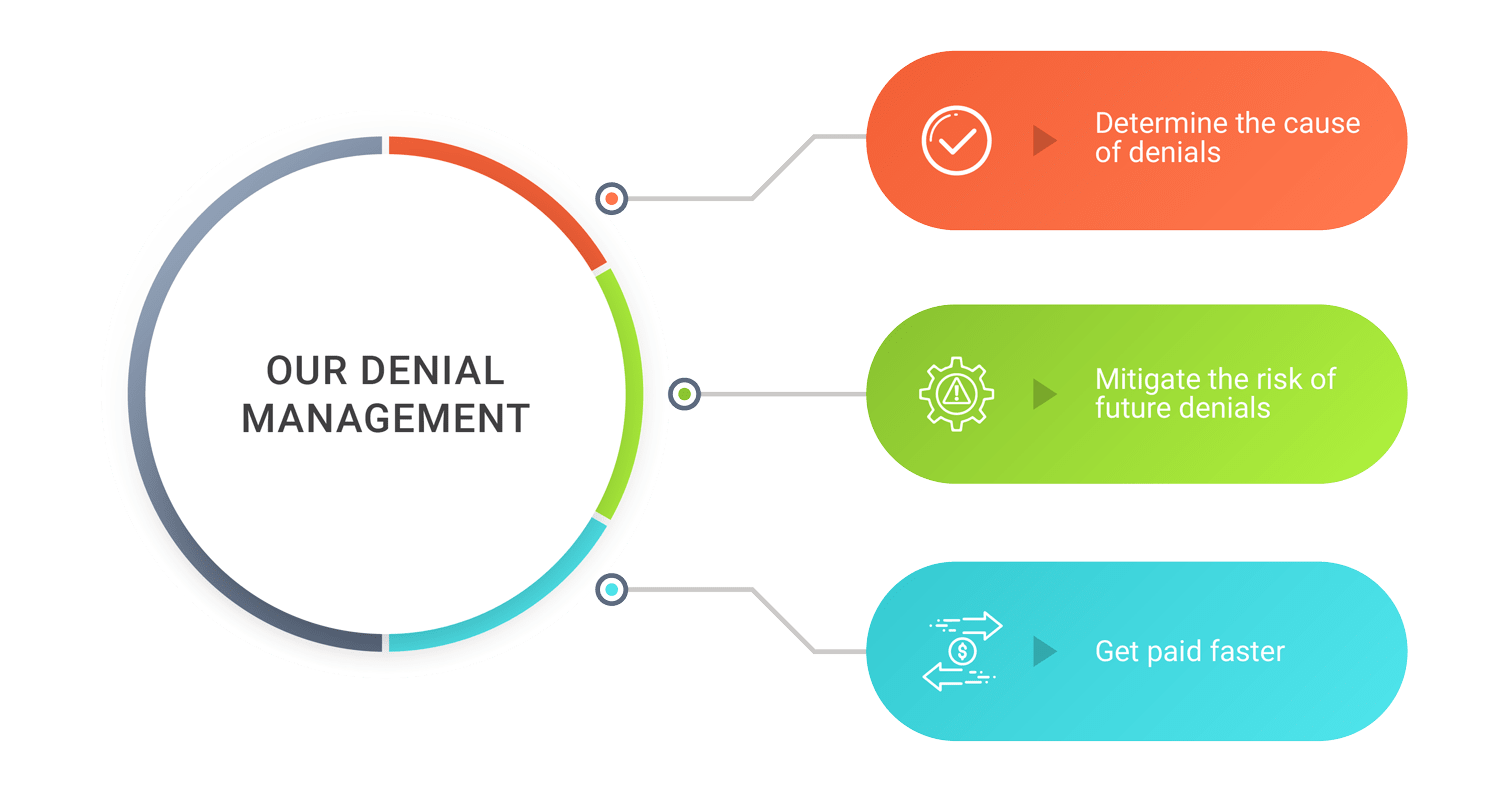
Denial Management

Dealing with medical claim denials is a time-consuming task and it’s a critical element in successful revenue cycle management. We follow a systematic, hands-on approach to deal with denied claims. As a first step, we analyse each claim and determine the best course of action. Secondly, we prioritize the claims based on patient demographics or business rules to ensure maximum benefits. Then, we take steps to prevent future denials by enhancing the billing practices in your healthcare.
We aim at the highest possible reimbursement on the claims. We help you maximize the success at collecting payments for denied / underpaid claims. Our systematic appeal process aggressively pursues reimbursement from contracted payers.
Let’s transform your revenue cycle today
When you create a high-performance revenue cycle, you’re finally free to invest your full resources into what matters most: the care of your patients.