Accounts Receivable Follow Up
Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
The accounts receivable follow-up team plays a crucial part as there are chances for the claims to get denied if they don’t adhere to the rules. Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
With our executive leadership team and highly skilled AR specialists, we proactively strategize the approach of denials received from payers. Our team will also work on fixing the clustered denials permanently to avoid delayed payments in future claims.
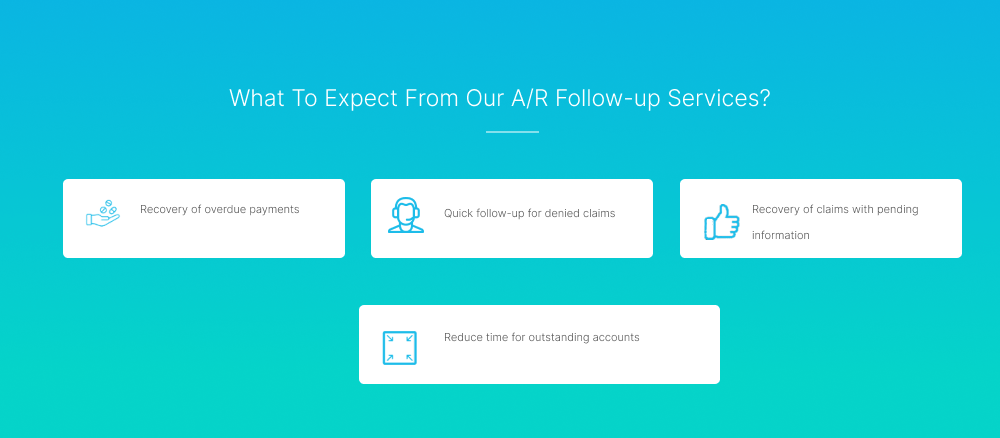
We strategize A/R follow-up through 3 phases
Initial Evaluation
In this phase, we identify and analyze the claims that are listed in the A/R aging report.
Analysis and Prioritizing
This phase is initiated when the insurance provider has not paid the rate agreed with the healthcare provider or when the claim marked as uncollectible is identified.
Collection
The claims that are identified within the filing limit are re-filed after verifying all the necessary billing information.
Let’s transform your revenue cycle today
When you create a high-performance revenue cycle, you’re finally free to invest your full resources into what matters most: the care of your patients.