RCM Services

Service Offerings
| Patient Access Services | Mid-Cycle Revenue Operations | Business Office Services |
|---|---|---|
| Appointment Scheduling | Encounter Documentation | Claims Management & Billing |
| Patient Registration | Coding | Payment Posting |
| Eligibility & Benefits Verification | Clinical Documentation Improvement | Accounts Receivable Management |
| Prior Authorizations & Pre-Certification | Charge Entry & Claim Audit | Denial Management |
| Patient Cost Estimation | Credit Balance | |
| Referral Management | Patient Statements | |
| Enrolment & Credentialing |
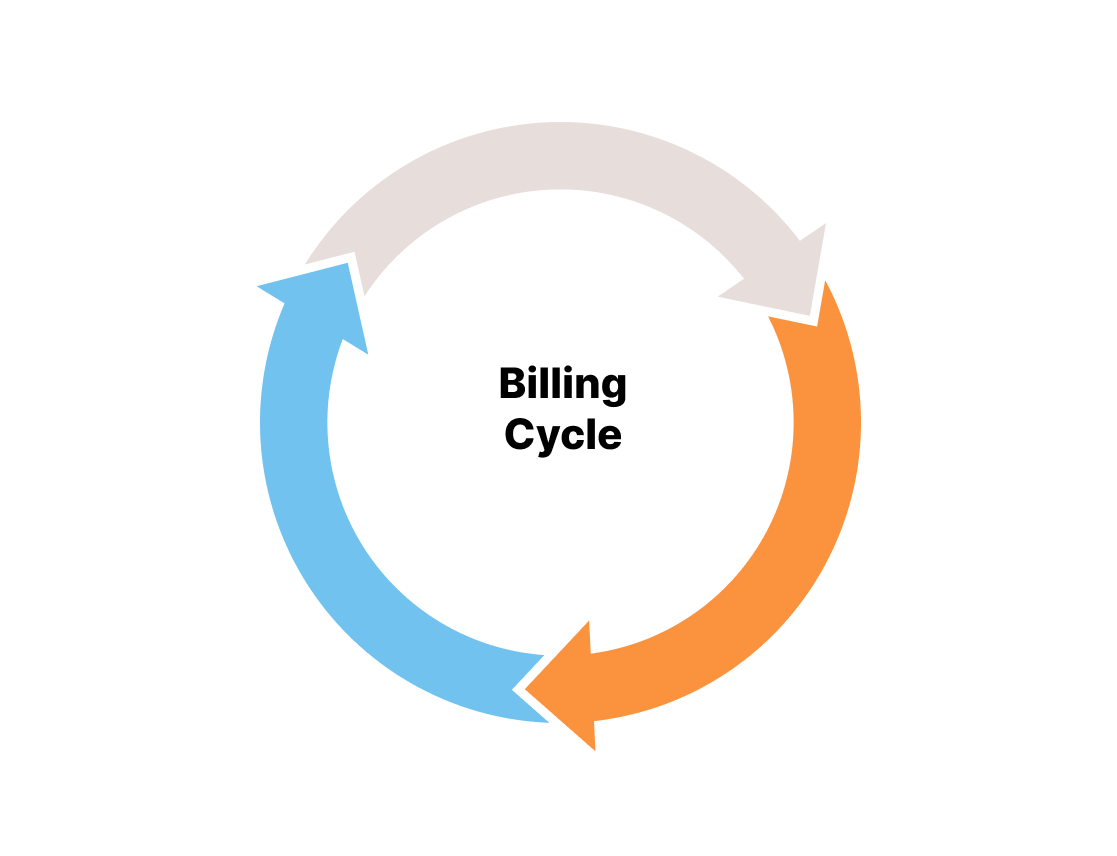
Pre-
Billing
- Patient intake Or scheduling appointment
- Eligibility verification & prior authorization
- Patient Registration or patient demographics
Post
Billing
- Remittance processing
- Accounts receivable
- Denial management
- Credit balance
Midterm
Billing
- Medical coding services
- Charge entry & claim audit
- Revenue integrity
- Medical coding review
- Clinical documentation compliance
Patient Registration
Like every aspect of healthcare, RCM begins with the patient. Similar to the payment and administrative aspects of healthcare, Patient’s input also plays a critical role. Getting complete and accurate patient’s information and capturing the information accurately into the revenue cycle system acts as a key success to revenue cycle management system
Eligibility & Benefits Verification
Accurate and timely determination of the patient’s eligibility is much needed to gather precise information regarding the patient’s insurance coverage. Such eligibility verification checks deliver an explicit view on patient's coverage, out-of-network benefits, and detailed insurance information.
Before the patient's visit to the healthcare provider, we ensure to conduct pre-insurance verification so as to verify the eligibility regarding the particular insurance.
Prior Authorization & Pre Certification
Prior Authorization plays a crucial role in RCM cycle as lack of authorization is a top driver in denials which jeopardizes the financial health of the healthcare organization.
Our prior authorization experts stay on top of each payer's ever changing requirments and manage the entire process of , including medical nessecity and referrals. Prior Authorizations are completed in real time.
Charge Entry
Revenue leakages can happen if efficient care is not put up for information documentation. In order to accomplish a sustainable improvement in the overall process, effective collaboration should be maintained between coding and charge entry teams.
Claims Submission
Wave Online also offers claim submission services to help the physicians rationalize their claims management. Our categorized style of passing on claims to specific payor groups based on pro-actively identified measures maximizes the efficiency of the claim submission process.
Payment Posting / Cash Posting
Payment posting is a resource-intensive task and a good payment posting team is responsible for the overall effectiveness of the revenue cycle process. Wave Online provides a streamlined payment posting workflow for insurance and patient payments. Our payment posting team do not just process payments, they provide insights on overpayment, denial, underpayment made. We also provide insights on clinical documentation and coding processes and effectiveness of your front-end patient collections.
Denial managemnet
Dealing with medical claim denials is a time-consuming task and it’s a critical element in successful revenue cycle management. We follow a systematic, hands-on approach to deal with denied claims. As a first step, we analyse each claim and determine the best course of action. Secondly, we prioritize the claims based on patient demographics or business rules to ensure maximum benefits. Then, we take steps to prevent future denials by enhancing the billing practices in your healthcare
Accounts Receivable Follow-Up
Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
The accounts receivable follow-up team plays a crucial part as there are chances for the claims to get denied if they don’t adhere to the rules. Our dedicated A/R team follows-up with the insurance provider to resolve denied claims. Appropriate actions are taken to receive maximum reimbursement from the insurance companies by reopening them.
Credit Balance
Once the insurance claim processing is over, our self-pay review team catch up with patients to identify if there are any funds to be received is in pending. Our self-pay review experts understand how critical it is to bill a patient, we ensure that a complete reconciliation of the patient payments before initiating a patient statement as per requirements (weekly/monthly), Further follow-up is performed through patient calls. If we don’t get a proper response from the patient, we recommend collections with a detailed report.
Reports
As a complement to our clients, Wave Online offers its reporting package for free. Our package contains detailed dashboards focusing on each sub-product we serve you, customized reports including insurance aging reports, Key Performance Indicators (KPI) report and payment cycle length report. It offers a detailed view of your practice's financial health. Our reporting capabilities and specialized analytics help your practice perform most granular level analysis for trends.
Let’s transform your revenue cycle today
When you create a high-performance revenue cycle, you’re finally free to invest your full resources into what matters most: the care of your patients.